Melanoma
What is melanoma?
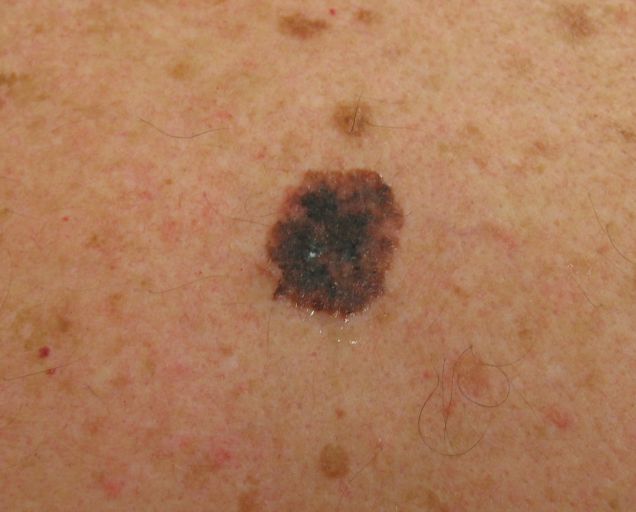
Melanoma is a cancer of the pigment-producing cells in the skin, known as "melanocytes". Cancer is a condition in which one type of cell multiplies without limit and in an unordered manner, while causing disruption to the function or replacement of normal tissues - almost like a wart. Normal melanocytes are found in the normal state in the outer layer of the skin, producing a brown pigment called melanin and whose function is to give the skin a shade. Melanoma is caused when melanocytes become cancerous, multiply and grow and invade other tissues. Melanoma often begins on the surface of the skin and at this stage it is easily visible and relatively easy to treat. If it is allowed time to develop, melanoma can grow inside the skin, until it reaches the blood vessels and lymph, through which it can metastasize, spread throughout the body and cause a life-threatening disease. The disease is curable when detected at an early stage, but becomes fatal if it is allowed to progress and spread out. Since once the disease has spread it is very difficult to treat it, the goal should be treatment as early as possible when the disease is still superficial on the surface of the skin. What causes melanoma? It is not known for sure what causes all types of melanoma. In any case, it is clear that excessive exposure to the sun, especially after severe sunburns, as far as blistering, in the first years of life there is an increased risk of melanoma formation. Ultraviolet radiation used in tanning salons has also been found to be related and may cause the outbreak of the disease. The tendency to have the disease also has a genetic background. Who does the disease affect? Anyone of any race and gender can get the disease, but fair-skinned people and those with sun-damaged skin are at a particularly increased risk. Since the main suspect in causing the disease is ultraviolet radiation from the sun, people who cannot tan or burn easily are at the highest risk. In addition to people who have been excessively exposed to the sun during their lives, people with multiple moles are also at risk. The average person has about 30 moles and they usually have no health significance. In contrast, people with more than 50 moles are at increased risk of contracting the disease. In addition to the number of moles, there are people whose moles are abnormal. These are known as "atypical moles" or "dysplastic moles" and they are also a marker for an increased risk of melanoma. In addition, the tendency to get the disease is inherited in families, and thus anyone who has a close relative who got melanoma, such as a parent, brother/sister, uncle/aunt, is also at an increased risk of getting the disease. Therefore, the following variables help to identify who is at increased risk of having the disease: Have fair skin Background of sunburn Over 50 moles unusual (atypical) moles A relative who had melanoma Anyone can get melanoma, but those who have one or more of the above-mentioned factors are at increased risk. Regular skin examinations, sometimes scheduled, by a dermatologist - can be life-saving in these cases! What to look for? Melanoma can appear anywhere on the skin and nails, including in places not directly exposed to the sun such as the eyes, mucous membranes (mouth and vagina) and internal organs. The most common locations in men are on the back and in women on the back of the calves. Melanoma is usually brown or black in color but sometimes in relatively rare situations it can be red, white or skin tone. It can start from a pre-existing mole or on skin that previously looked completely normal. Melanomas grow slowly, so any lesion that appears to be growing or changing should raise suspicion. When looking for birthmarks/moles on the skin, look for the signs of age spots: Geometry - the shape of the mole is not symmetrical, one half is not equal to the other half. Border - a mole whose border is not rounded, clear and defined. Shade - a mole whose color is not uniform and consists of several shades such as: brown, black, pink and more. Size - a mole whose diameter exceeds 5 mm (the diameter of a pencil). Height - a point that was flat and developed a "hump". Development - changes in size, color, bleeding, itching, etc. What is the treatment? The best treatment is early detection and removal. A thorough examination by a dermatologist, preferably with the help of dermoscopy, can diagnose whether a certain lesion is suspicious or not, and if so, the next step is a biopsy or excision of the lesion. The lesion area is anesthetized, and the entire lesion or a piece of it is sampled and submitted for pathological examination using the microscope. Confirming the diagnosis through the microscopic examination, it is possible to determine the depth of the lesion and where the tumor has penetrated the skin, and based on this data, the continuation of the treatment is decided. The treatment begins with a repeated and extensive excision of the margin of the healthy skin around the lesion, the purpose of which is to ensure that no remnants of the tumor remain in the patient's skin. Early melanoma that is limited to the outermost layer of the patient's skin is called Melanoma in situ and its complete excision yields a 100% cure! If the melanoma is not removed and allowed to grow and penetrate deep into the skin - the melanoma becomes a life-threatening disease due to the risk that it will reach blood vessels or lymph vessels and send metastases through them to other sites in the patient's body. Usually when melanoma spreads it first reaches the lymph nodes that drain the area of the skin where the melanoma is located. The lymphatic system, of which the glands are a part, is a system of piping that drains fluids from the tissues and its function is to clean the tissues and monitor their condition through the immune system. In melanomas deeper than 1 mm and in melanomas with additional features that increase the risk that they have metastasized, it is customary to perform a test in which a special marker is inserted into the site where the melanoma was discovered in the skin. The marker travels through the lymphatic system to the group of lymph nodes responsible for the area and thus it is possible to perform what is called "Sentinel node biopsy" - this is the first lymph node of the group of glands that the marker reaches. This gland is removed and sent for examination, and if it does not contain tumor cells, this is a good indication that the tumor has not yet metastasized. Early detection and diagnosis of melanoma is the most effective treatment for the disease and this is the role of dermatologists. After the resection of the tumor, the continuation of the treatment of patients with invasive melanoma goes to oncologists who specialize in the oncological treatment of the disease. At this stage, the role of the dermatologist is preventive monitoring - for the early detection of additional melanomas, should they appear. In recent years, mutations have been discovered in the genes responsible for the growth rate of cells in melanoma tumors, and following the discovery of the proteins produced by these genes, new drugs called "biological" were developed because their action is to interfere with the biological pathways and not to poison the cells (unlike chemotherapeutic drugs). These discoveries constitute a great revolution in treatment in melanoma and although they only appeared in recent years, it is already clear that they are capable of significantly prolonging the lives of melanoma patients, even in those suffering from widespread and even metastatic disease. More tests? A complete physical examination of the patient's body and an eye examination must be performed. Depending on the depth of the tumor and the findings of the sentinel gland biopsy, it is customary in some cases to also perform imaging tests such as whole-body CT, MRI and/or PET mapping, whose role is to identify, if possible, already existing metastases. After the evaluation - if it turns out that the tumor has already metastasized - a treatment plan is tailored for each case, which may include surgical excision of metastases, chemotherapy, immunotherapy or radiation is adapted to each case. How can the disease be prevented? Since the main suspicion of causing the disease is the ultraviolet radiation from the sun - it is very important to protect yourself carefully from the sun's radiation. Avoid being in the sun during the hours of peak radiation between 9.30 am and 4 pm. Apply a broad-spectrum sunscreen that prevents the penetration of both UVA and UVB radiation and re-apply it every two hours. Make sure to wear a wide-brimmed hat, sunglasses, and Clothing from a dense fabric that protects against the penetration of the sun's rays. Artificial tanning should be avoided. Early detection remains the best treatment, so you should learn and perform self-examination regularly (preferably once a month) to look for changes in the color, size or shape of the skin moles or the appearance of new moles. In case of an unusual finding or a change in an existing lesion, you should contact a dermatologist to check and diagnose the finding as soon as possible. In addition, it is recommended to adhere to a regime of regular examinations by a dermatologist - at least once a year or more if the doctor thinks that a higher frequency is necessary. The article is provided as a public service. In Dr. Gilead's clinic, follow-up tests are performed on patients at increased risk of melanoma using dermoscopy and photographic documentation of suspicious moles and lesions. Patients are subjected to a thorough physical examination at a frequency determined by the degree of risk in which the subject is and the number of moles. Follow-up by photographing each mole will be performed as part of a Private visit, paid separately. It should be emphasized that the treatment of patients with invasive and/or metastatic melanoma after the discovery and resection of the primary tumor is performed by oncologists who specialize in this and Dr. Gilead has not specialized in this area of treating the disease.


